mRNA vaccines: let's eradicate herpes, cure cancer, and be sick a whole lot less
Quick, inexpensive, made-to-order treatments
Is there a healthcare topic you’d like to see covered, or a health question you need answered? Leave a comment or send me a message and the next article may be written especially for you!
You’re probably infected right now (the problem of pathogenic persistence)
I ended “The unexpected gift of Long COVIDLong COVID: could new research treat chronic fatigue syndromes and cure cancer?” by saying that even though Post-Acute-Infectious-Syndromes (PAISes) like Long COVID can be caused by a wide variety of pathogens (viruses, bacteria, fungi, parasites, bad vibes from that annoying girl you knew in college), we probably don’t have to treat the pathogen itself to treat the PAIS. Research shows significant overlap in the pathways causing chronic symptoms, even if the initial triggering pathogen is unknown. It’s likely that multiple pathogens are responsible for triggering the same PAIS symptoms. If, say, 10 different bacteria, 15 viruses, and 2 fungal infections all trigger a biochemical pathway that causes a leaky blood-brain barrier, which, in turn, causes the symptom of “brain fog,” then one treatment for “blood-brain barrier problems” might work well.
As with Long COVID, pathogens can trigger pathways that stay triggered even after the body has defeated the pathogen. For example, you get COVID, then your body eliminates COVID, but the symptoms of Long COVID persist because the initial infection triggered pathways that lead to fatigue, brain fog and heart rhythm abnormalities. The virus is gone, but the PAIS, annoyingly, remains.
Creating drugs that address the pathway leading to “leaky blood-brain-barrier problems” rather than the individual pathogen triggering the pathway (which could potentially be triggered by hundreds of pathogens!) will likely mean more treatments, faster, for more people, especially if a common blood biomarker—a chemical in the blood that signals that a certain pathway has been triggered—can be identified and tested for.
Anything that helps more people get treatment faster is good for human flourishing, but being able to use single therapies against multiple disease types is especially important because the FDA is so painfully slow, and so indifferent to human suffering. It takes, on average, eight years to get a new drug through clinical trials.
As I mentioned briefly at the end of part 1, the problem is that drugs treating pathways triggered by otherwise defeated pathogens won’t work if symptoms are caused by pathogens that actually remain in the body (otherwise known as "pathogenic persistence”). Pathogenic persistence means that the body can’t eliminate the pathogen (the virus, bacteria, fungus or parasite) after becoming infected. Treating the pathways these pathogents triggermight help, but if you stop treating the pathway, symptoms are likely to come back, because the pathogen is still there. It’s like buying increasingly expensive presents for a girlfriend you want to marry, but who won’t commit to you. Maybe she seems temporarily more loving after you give her a fancy bauble, but until you break it off and pull the knife from your heart, you’re going to keep bleeding.
Persistent viral infections are common (you probably have one right now) and the cost of persistent viral infections is high—and high in ways scientists and doctors didn’t appreciate for a long time. Some examples, as previously noted:
· Epstein-Barr Virus (EBV) is a major risk factor in the development of multiple sclerosis (30-fold increase in risk), lymphoma, and nasopharyngeal cancer. It may play a role in other cancers, such as breast cancer. Ninety-five percent of adults carry EBV. Epstein-Barr is sneaky. It actually encodes small RNAs (which are information the body uses to make proteins) that can inactivate genes that are stimulated by a normal immune response. This is similar to the way mRNA vaccines work: by introducing RNA into the body, so that cells can read the RNA, which teaches those cells how to make proteins, which then exert the desired effect. EBV is making its own RNA “vaccine” to exert the desired effect of evading the immune system.
· Human Papilloma Virus (HPV) infections are implicated in cervical, anal, oral and genital cancers. Fortunately, we have a vaccine. Unfortunately, too few people get it.
· Herpes Simplex Virus (HSV) may play a major role in Alzheimer’s. Up to 80% of adults have an HSV1 infection. HSV1 and HSV2 are poxviruses that live in nerves forever. Chicken Pox (varicella) is also a persistent poxvirus that lives in nerves. Reactivated varicella virus becomes a shingles rash.
· Lyme disease may have a long tail of weird symptoms, and its ability to hide inside the cells lining blood vessels may help it evade the immune system and create a persistent infection. Tragically, we had a working Lyme disease vaccine that the company pulled due to anti-vaxxer hysteria.
To address viral persistence, vaccines, especially mRNA vaccines, are our best bet for speed and flexibility. Preventing infection in the first place is ideal, but vaccines can also help improve the response against an infection, thus reducing the risk of pathogenic persistence, or help to reduce the amount of pathogen that persists inside the body.
Why mRNA vaccines, where other vaccines have failed?
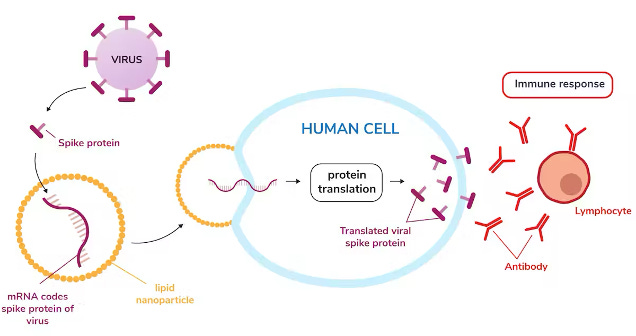
Consider how mRNA vaccines work: Messenger RNA (mRNA) is a molecule that contains instructions that tell cells how to make various proteins. Each protein has its own novel set of RNA instructions. All proteins made in a human body are built when a cell “reads” the RNA instructions.
An mRNA vaccine synthesizes mRNA instructions in a lab using uniquely organized strands of just four building block chemicals called nucleotides: Adenine, Cytosine, Guanine and Uracil. Varying combinations of these four molecules can instruct the body to create basically any protein. These instructions are read inside a cell, and the protein is made by the cell.
RNA is fragile. So, like in the COVID mRNA vaccines, these instructions can be delivered in a protective fatty bubble called a “lipid nanoparticle.” Think of it like a balloon made of fatty acids, with the instructions nestled inside. Once injected, these lipid nanoparticles take the mRNA instructions into cells, where the fatty bubble degrades, mRNA instructions are released, and the cell’s machinery start to produce whatever protein the mRNA tells it to.
For COVID, the mRNA instructed the cells to make the spike protein, which is found on the outside of the COVID virus. But we can make mRNA vaccines that teach a cell to make any protein that corresponds to a protein on a pathogen that doesn’t normally exist in the human body. Once the cells started making the spike protein, or any protein the body doesn’t normally use, the body’s immune system recognizes the protein as foreign, and mounts an immune response against it. This is how the body creates antibodies, which act like immune memory. The immune system mounts a response just as it would if that protein was introduced to the body by a pathogen, except with the vaccine, your body learns to recognize parts of the pathogen without ever being infected.
Why are mRNA vaccines the future?
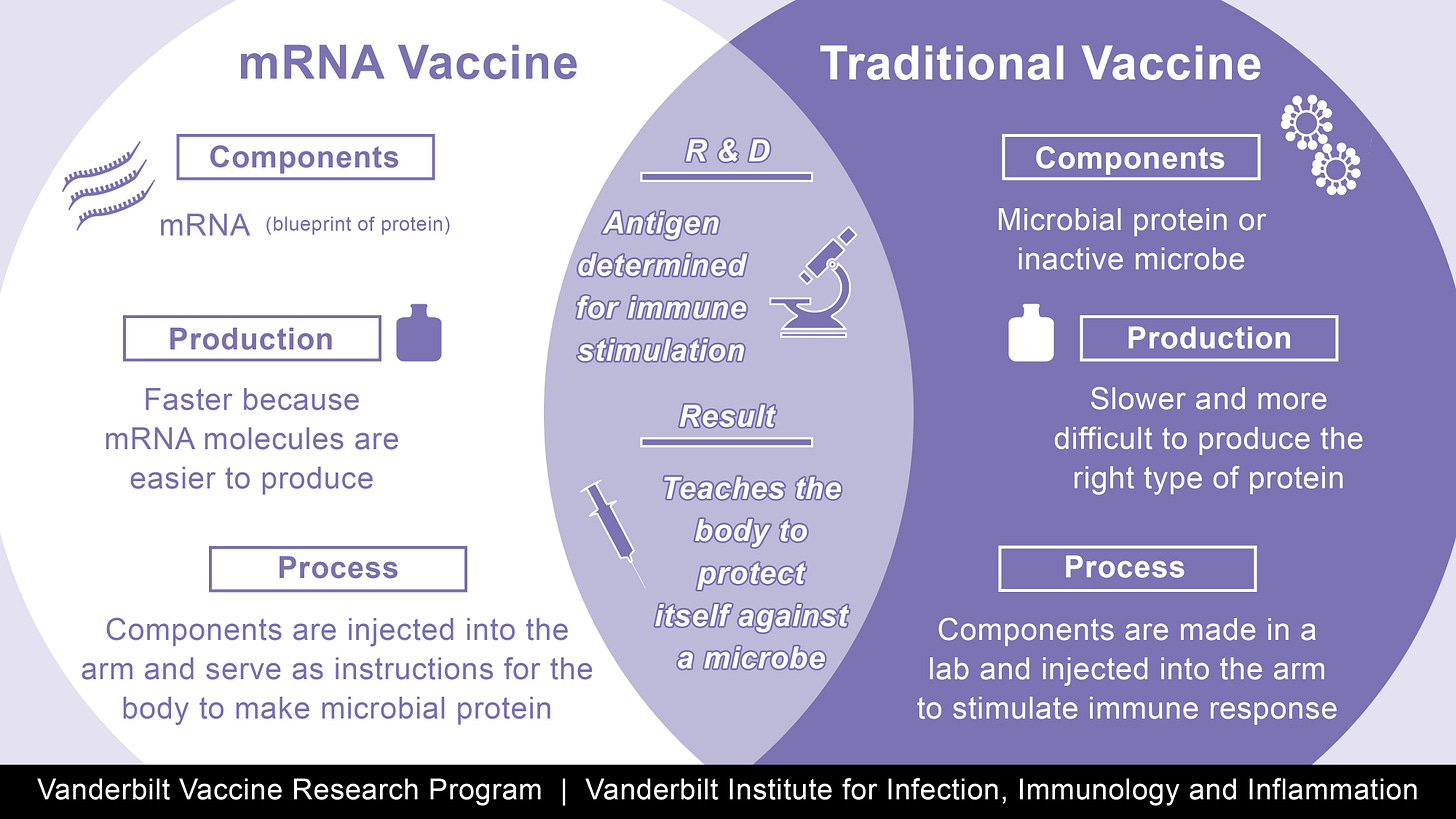
MRNA vaccines are faster, cheaper and more flexible to make than their traditional counterparts:
· Synthetic mRNA, the foundation of the vaccines, can be designed and manufactured in a lab within days of the sequencing of the genetic code of a pathogen’s target protein.
· MRNA vaccines don’t rely on growing large quantities of weakened virus or viral vectors, which eases production.
· They’re flexible: Since cell cultures (imagine test tubes filled with animal cells that are infected with a virus and used to grow large quantities of the virus ) aren’t necessary, and the mRNA instructions can be quickly synthesized in a lab, if there is a mutation in the virus, it’s much quicker and easier to create new mRNA vaccines. New mutations? Re-create the new target protein in the lab. mRNA vaccines are the Burger King of vaccines: you can have it your way.
· MRNA vaccines can code for multiple protein targets on a single virus, which means that they can better address resilient pathogens resistant to vaccine development, like herpes . Attacking multiple protein targets at once might create a more robust immune response. MRNA vaccine trials for genital herpes, which traditional vaccines have failed to prevent, are currently underway with BioNTech. That’s great news for prevention.
MRNA vaccines have the potential to prevent future infection from so many pathogens that plague us, but what about people who are already infected? Eighty percent of American adults already have herpes virus type 1, and 95% of the adult population ages 35+ carry Epstein-Barr Virus (EBV). MRNA vaccines might act to modulate the body’s downstream response to a virus, even after infection.
HPV is a good proof of concept regarding the possibility that vaccines can decrease negative downstream effects of an infection, even if it’s too late to prevent an infection. Studies show that HPV-vaccine naive patients who are HPV positive, with early precancerous cervical changes (“CIN1”), and who receive the HPV vaccine after diagnosis, have a decreased progression of precancerous changes (CIN2,3). HPV vaccination provides a pathway for both infection prevention and decreased effects of persistent infection. That the vaccine seems able to head off cancer is important in light of how many women and men don’t get the vaccine when they should. Still, between 2012-19, cervical cancer incidence in women in their 20s decreased by 65%, despite poor vaccine uptake. Preventing HPV decreases cancer risk, but so does, to a lesser extent, receiving the vaccine after infection. That’s great news for women who didn’t receive the vaccine due to fear or age. And it’s great news for men, since HPV can cause oral, neck, penile, and anal cancers. HPV decreases the amount of fun in the world and the vaccine increases it. Science rules!
Quick aside: Right now, the HPV vaccine is “approved” up to age 46, but that’s mostly based on arbitrary age cutoffs chosen for the initial studies and the belief that a person needs to be vaccinated before they’re exposed for benefit. Nothing indicates that the HPV vaccine is dangerous for people over 46, and the age cutoff was chosen based on the frankly wrongheaded and naive assumptions about the sex lives of women (and men) who are married or over a certain age. Assuming that age or marital status will prevent someone from HPV exposure assumes that people are having less sex as they age, monogamous sex, and ignores the 107% uptick in STIs among patients over 55+ in the last decade. If you’re a human being who hasn’t had the HPV vaccine and you have ever been sexually active or are currently sexually active, or will be sexually active, get the series or a booster.
Is there viral persistence in Long COVID?
Sometimes. Patients have been found to be COVID positive for months after their initial infection on antigen tests, which are looking for active infection, and not antibody tests, which look for past infection. Viral persistence increases the risk of Long COVID.
COVID vaccination appears to confer a 40-60% reduction in Long COVID. Studies suggest that vaccines might have both protective and therapeutic effects on LLong COVID. Therapeutic effects, by which I mean giving a person with Long COVID a COVID vaccine and seeing their Long COVID symptoms decrease, makes me wonder if viral persistence is a bigger overall problem in COVID than we’ve realized.
Vaccine skepticism hurts in terms of uptake (thanks, Wakefield—he’s the guy who made up data that first spread the “vaccines cause autism” meme). The initial conversation around COVID vaccination revolved around preventing deaths, but it’s clear that, as a society, we’ve decided that COVID deaths are allowable background noise. But, beyond death itself, there are also tremendous human misery and socioeconomic costs from a huge uptick in chronic illness and disability.
MRNA vaccines as personalized cancer cures
Think of mRNA vaccines as injectable instructions that turn your body’s cells into factories that can create any protein for which mRNA instructions can be built. Because a researcher can theoretically make mRNA instructions for any protein, mRNA vaccines aren’t only useful against pathogens; they can be used to teach the body to mount an immune response to any foreign protein that you want destroy, including proteins on cancer cells—called neoantigens—caused by mutated tumor DNA.
To create an mRNA cancer vaccine, a patient’s tumor is biopsied to identify unique target mutations —> mRNA correlating to mutations is synthesized and injected into the patient —> the patient’s cells create the targeted protein —> the creation of foreign proteins stimulates the immune system and teaches it how to recognize the target protein —> The immune system (especially T cells) search for this target protein and destroy the cancer cells to which it’s attached. Cancer cells are notorious at finding ways to hide from the immune system, but the mRNA vaccine is like giving the immune system magnifying glasses. The mRNA cancer vaccine production process is similar to that of producing a COVID vaccine, except, instead of a spike protein, the target is the neoantigen. Thanks to the speed and flexibility of mRNA vaccines, everyone with cancer could have a personalized cancer vaccine that’ll have significantly fewer side effects than chemo or radiation.
R&D for the mRNA COVID vaccines has already hastened the development of mRNA cancer vaccines. Foundational mRNA research focused on cancer: Ozlem Tureci, MD, co-founder and CMO of BioNTech, performed research in mRNA-based cancer therapies and also led the clinical development for “Project Lightspeed” to develop an mRNA COVID vaccine. Drew Weissman’s lab at U Penn created the platform for nucleoside-modified mRNA-lipid nanoparticle vaccines, which Pfizer, BioNTech, and Moderna used for COVID vaccine development. Weissman’s lab also works on ways to use mRNA vaccines in bone marrow stem cells and T cells.
The most exciting mRNA cancer vaccine study Is currently Moderna’s 4157 vaccine for melanoma, lung cancer, head and neck cancer, and probably others. Patients with high-risk stage III/IV melanoma had a complete resection of their tumors followed by mRNA-4157 and the immune checkpoint inhibitor Keytruda, or Keytruda and placebo injection. MRNA-4157 and Keytruda reduced the risk of recurrence or death by 49%, and the risk of distant metastasis or death was reduced by 62% compared to Keytruda alone. This year, Moderna is expanding clinical trials to patients with non-small cell lung cancer. Phase 1 studies also showed extremely promising results in notoriously difficult-to-treat head and neck cancer, with two of the ten patients having complete resolution of their tumors, and 40% having a significant, if partial, response. Late-stage and recurrent head and neck cancer
Bespoke immunotherapy tailored to a patient’s exact tumor will change the way cancer is treated. Immunotherapies don’t yet work for all cancers. Moderna’s mRNA-4157 fell short for colorectal cancer, but there are other companies like Genentech also working on colorectal cancer. Genentech is currently running a phase 2 open-label study for pancreatic cancer. FDA requirements are slowing down progress—Moderna apparently can’t get approval until they have their factory ready. Delay means more cancer patients will be added to the invisible graveyard), but progress is at least being made. COVID showed us how fast we can progress, and I hope that researchers keep up the pace in applying mRNA vaccines across pathogens and cancers.
The need for both mRNA technology and speed is deeply personal, and not just because I’m a physician who wants to offer her patients better treatments: my husband Jake has recurrent metastatic head and neck cancer. He’s being kept alive by a clinical trial drug, petosemtamab, but there isn’t a standard-of-care option that can cure him. Squamous cell carcinoma recurrence and metastases is a death sentence, unless, maybe, his immune system can be trained to mount a targeted, sustained response. Only about 20 – 30% of head and neck cancer patients like Jake respond to Keytruda alone or Keytruda combined with chemo. Moderna’s mRNA-4157 vaccine might change the whole head and neck cancer game. There’s rumor that Moderna might expand their phase 2 studies to include additional cancer types this year, and, if anyone from Moderna’s reading this, we’re in Arizona, close to the site where you ran the phase 1 head and neck study, and Jake will be the first patient to sign up.
At the beginning of the pandemic, I feared I’d bring home COVID from the hospital and accidentally kill Jake. Now, COVID and mRNA development might be the impetus for the treatment that keeps him alive.
In the way wars accelerate technological and medical developments, so, too do pandemics, which are themselves a kind of war. Four years in, physicians have learned a lot about human suffering. Now, I’m hopeful that the ongoing lessons of COVID might change the way we perceive, diagnose, and treat chronic illness, PAISess, and cancer. The momentum we’ve built is precious, and proof that science and research can happen quickly when adequately motivated. I hope we keep up the pace, even as the FDA slows progress and We’ve paid dearly for COVID’s gifts. Let’s not squander them.
If you’ve gotten this far, consider the Go Fund Me that’s funding my husband Jake’s ongoing cancer treatment.





This is the finest teaching material on a difficult subject that I've seen.
Thank you, Dr. Stillman - not only for this post, but for sharing your life and love through your dedication and commitment to serve.
Since the mRNA carrying lipid nanoparticles can and do go anywhere in the body including across the blood brain barrier, what enables them to be targeted to only cells that would be potentially beneficial to turn into spike or other protein factories? How long are cells acting as these factories? What turns off that mechanism?